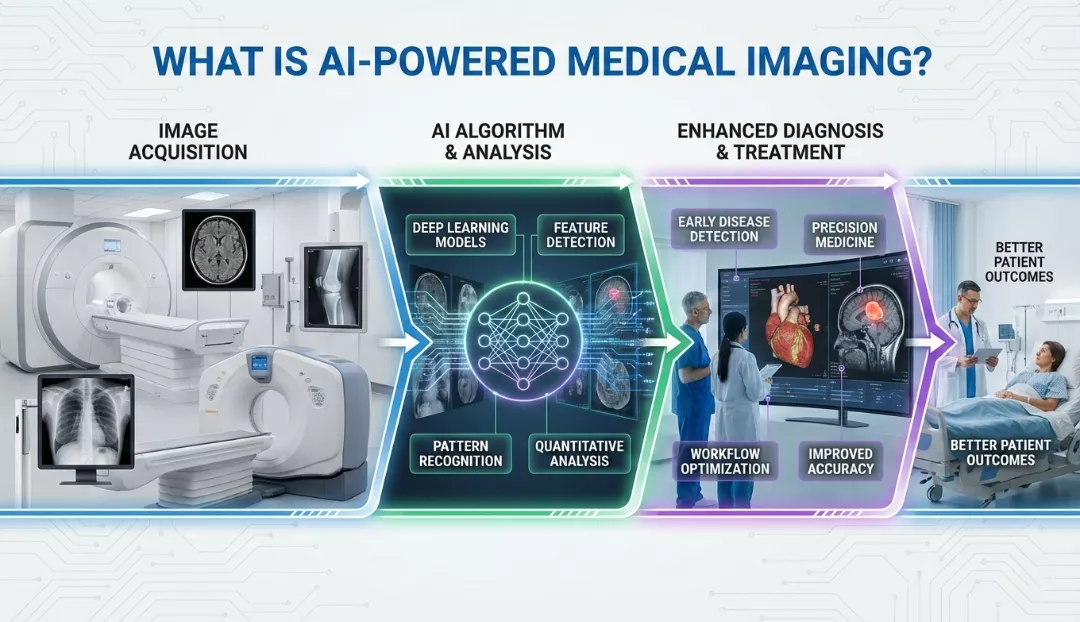
AI-powered medical imaging refers to the use of artificial intelligence, specifically machine learning (ML) and deep learning (DL) algorithms, to analyze medical images such as X-rays, CT scans, MRIs, and ultrasounds for improved diagnostic accuracy and efficiency. Unlike traditional imaging which relies solely on human interpretation, AI systems are trained on vast datasets of annotated images to automatically recognize complex patterns, detect anomalies (like tumors or fractures), segment anatomical structures, and quantify disease progression with pixel-level precision.
This technology functions as a “second pair of eyes” for radiologists, helping to prioritize urgent cases, reduce diagnostic errors, and predict patient outcomes based on imaging biomarkers that may be invisible to the human eye.
Introduction: The New Era of Diagnostics
The integration of Artificial Intelligence (AI) into healthcare is not just a futuristic concept—it is a rapidly expanding reality that is fundamentally reshaping how diseases are detected and treated. Medical imaging, the cornerstone of modern diagnostics, generates petabytes of data annually. Radiologists and pathologists are often overwhelmed by the sheer volume of scans, leading to fatigue and potential burnout.
AI-powered medical imaging steps in as a transformative solution. By leveraging advanced computational models, healthcare providers can now process images faster, diagnose with higher confidence, and offer personalized treatment plans. This guide offers a comprehensive look at the technology, applications, benefits, and future of AI in medical imaging.
How AI-Powered Medical Imaging Works
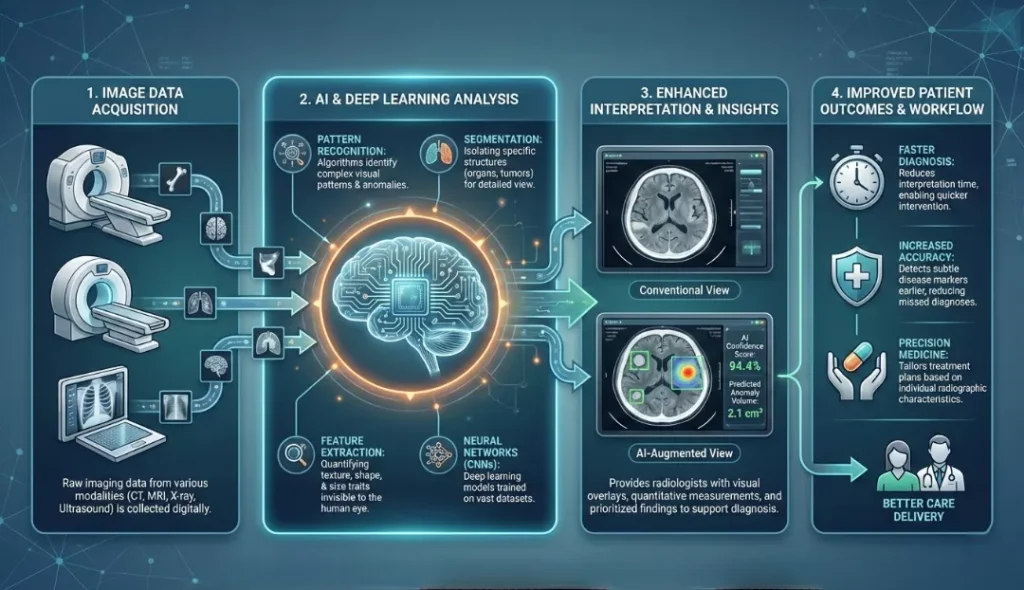
To understand the “magic” behind the technology, we must look at the underlying engines: Machine Learning (ML) and Deep Learning (DL).
1. The Role of Deep Learning and CNNs
At the heart of modern medical imaging AI is a type of deep learning architecture called the Convolutional Neural Network (CNN). CNNs are designed to mimic the human visual cortex.
- Input: The system receives a medical image (e.g., a chest X-ray).
- Feature Extraction: The network breaks the image down into layers, analyzing edges, textures, and shapes.
- Classification/Segmentation: The AI identifies specific features—such as a nodule in a lung or a blockage in an artery—and classifies them based on probability.
2. Training the Algorithms
AI models do not “know” medicine; they learn it. Developers feed the algorithms thousands (sometimes millions) of labeled images—for example, “healthy brain” vs. “brain with glioblastoma.” Through iterative training, the model adjusts its internal parameters to minimize errors, eventually achieving accuracy rates that often match or exceed human experts in specific tasks.
Key Applications Across Medical Specialties
AI is not a one-size-fits-all tool; its application varies significantly across different medical fields.
Radiology: The Frontline of AI Adoption
Radiology has seen the highest adoption rate of AI, accounting for approximately 75% of all FDA-approved AI medical devices.
- Triage and Prioritization: AI algorithms can scan incoming ER images (like CT head scans) to detect intracranial hemorrhages or strokes. If a critical issue is found, the scan is flagged to the top of the radiologist’s worklist.
- Fracture Detection: AI tools assist in identifying subtle fractures in X-rays that might be missed during a busy night shift.
Cardiology: Visualizing the Heart
- Echocardiography: AI automates the measurement of the heart’s chambers and ejection fraction, reducing the manual time required by sonographers.
- Blood Flow Analysis: specialized algorithms analyze non-invasive CT scans to model blood flow in coronary arteries, potentially replacing invasive angiograms.
Neurology: Time is Brain
- Stroke Management: In acute stroke cases, AI software (like Viz.ai) analyzes CT angiograms to detect large vessel occlusions and alerts the neurovascular team in real-time, significantly reducing “door-to-needle” time.
- Alzheimer’s Prediction: AI models analyze metabolic changes in PET scans to predict the onset of Alzheimer’s disease years before clinical symptoms appear.
Pathology and Oncology
- Digital Pathology: AI scanners digitize glass slides, allowing algorithms to count cancer cells (mitosis counting) and grade tumors more consistently than human pathologists.
- Radiomics: This emerging field uses AI to extract quantitative features from medical images that are invisible to the naked eye, helping to predict how a tumor will respond to immunotherapy or radiation.
Recent Statistics and Market Trends (2024–2026)
The growth of AI in medical imaging is supported by compelling data. The market is shifting from “experimental” to “essential.”
Market Size and Growth
- Global Market: The global AI in medical imaging market was valued at approx $1.28 billion in 2024 and is projected to skyrocket to over $14 billion by 2034, growing at a CAGR of roughly 27-30%.
- Adoption Rates: A recent survey indicates that nearly 30% of radiology practices in the US have implemented some form of AI tool as of 2025.
FDA Approvals and Efficiency
In 2024 alone, the FDA authorized a record number of AI/ML-enabled medical devices, the vast majority being in radiology.
Impact of AI on Medical Imaging Efficiency (2024-2025 Data)
| Metric | Traditional Workflow | AI-Augmented Workflow | Improvement |
| Stroke Detection Time | 60+ minutes (scan to alert) | < 5 minutes (scan to alert) | 90%+ Faster |
| Radiologist Reporting Time | 15-20 mins per complex case | 10-12 mins per complex case | ~25% Efficiency Gain |
| False Positive Rate (Screening) | Higher variability | Reduced by up to 60% | Higher Specificity |
| Nodule Detection Sensitivity | ~75-85% (Human eye) | ~95-99% (AI + Human) | Early Detection Boost |
Note on ROI: Healthcare organizations are seeing a Return on Investment (ROI) of approximately $3.20 for every $1 invested in AI technologies, primarily driven by operational efficiency and reduced malpractice risks.
Benefits of AI-Powered Imaging
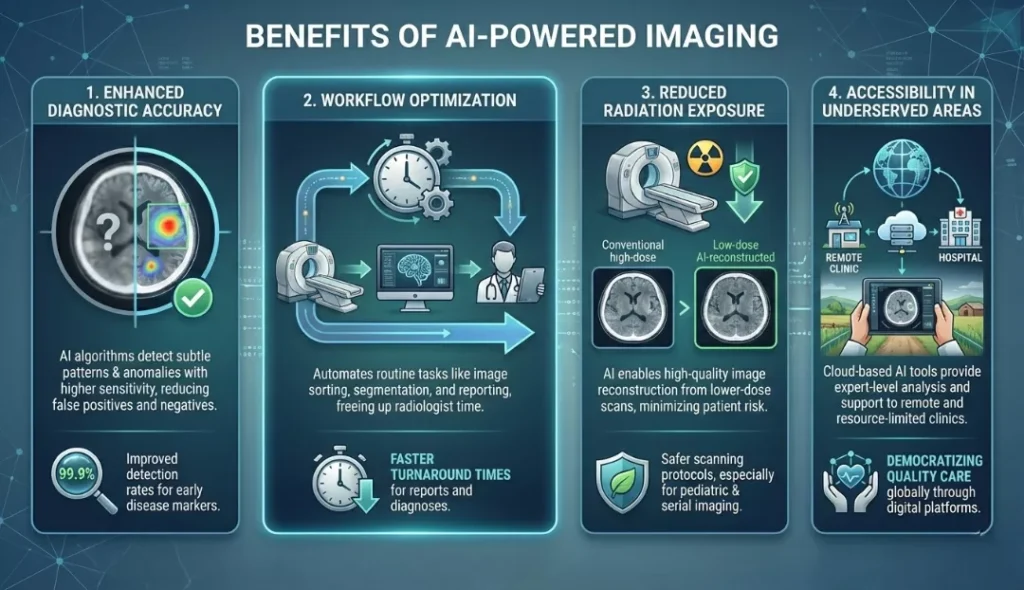
- Enhanced Diagnostic Accuracy: AI eliminates the “satisfaction of search” error, where a radiologist stops searching after finding one abnormality. AI scans the entire image pixel-by-pixel, ensuring secondary findings (incidentalomas) are not missed.
- Workflow Optimization: By automating tedious tasks—such as measuring tumor diameters or counting cells—AI frees up physicians to focus on complex decision-making and patient interaction.
- Reduced Radiation Exposure: AI algorithms can reconstruct high-quality images from low-dose CT scans. This allows hospitals to reduce the radiation dose given to patients (especially children) without compromising image quality.
- Accessibility in Underserved Areas: Portable ultrasound devices equipped with AI guidance enable non-experts in rural areas to capture diagnostic-quality images, which are then analyzed by the AI or sent to a remote specialist.
Challenges and Ethical Considerations
Despite the optimism, significant hurdles remain before AI becomes ubiquitous.
- Data Bias and Generalizability: An AI model trained mainly on data from one demographic (e.g., Caucasian males in the US) may perform poorly when analyzing images from a different demographic due to biological variances. This “algorithmic bias” is a major focus of current research.
- The “Black Box” Problem: Deep learning models are often opaque; it is difficult to understand why the AI made a specific diagnosis. In medicine, “explainability” is crucial for trust.
- Integration Hurdles: Hospitals use legacy IT systems (PACS/RIS). Integrating modern AI tools into these old frameworks can be technically difficult and costly.
- Liability: If an AI misses a diagnosis, who is responsible? The software developer, the hospital, or the supervising radiologist? Legal frameworks are still evolving to answer this.
The Future: What to Expect (2025–2030)
The next five years will move beyond simple detection to predictive and generative capabilities.
Generative AI in Imaging
Generative AI (like the tech behind ChatGPT, but for images) will be used to create “synthetic” medical data to train models without compromising patient privacy. It will also help in “image-to-image” translation, such as converting an MRI scan into a CT-like image for radiation planning.
Multimodal AI
Future systems will not just look at the image. They will be multimodal, analyzing the X-ray alongside the patient’s genetic data, electronic health records (EHR), and lab results to provide a holistic risk assessment.
Opportunistic Screening
AI will run in the background of every scan to check for silent killers. For example, a patient undergoing a CT scan for a kidney stone might be automatically screened for osteoporosis or aortic calcification (heart disease risk) without any extra cost or radiation.
Conclusion
AI-powered medical imaging is not about replacing doctors; it is about replacing the limitations of human perception. By handling the repetitive, quantitative, and pattern-recognition tasks, AI empowers healthcare professionals to practice at the “top of their license.”
As we move through 2026 and beyond, the collaboration between human expertise and artificial intelligence will become the standard of care, leading to earlier diagnoses, more precise treatments, and ultimately, saved lives. For patients and providers alike, the message is clear: AI is the stethoscope of the 21st century.
Check Also: AI in Drug Development: How Artificial Intelligence Speeds Discovery
Frequently Asked Questions (FAQs)
1. Will AI eventually replace my radiologist or doctor?
No. Think of AI as a smart assistant, not a replacement. AI is excellent at spotting patterns and measuring data, but it lacks human empathy and clinical judgment. It handles the repetitive work so your doctor can focus on you. As the saying goes: “AI won’t replace radiologists, but radiologists who use AI will replace those who do not.”
2. Is AI 100% accurate?
No tool is perfect, which is why we use a “Human-in-the-Loop.” AI is incredibly good at finding subtle issues (like early-stage lung cancer), but it can still make mistakes. That is why a certified radiologist always reviews the AI’s findings. The AI flags potential issues, and the human expert makes the final call.
3. Is my personal health data safe?
Yes, your privacy is the top priority. Before any AI analyzes your images, your data undergoes de-identification. This strips away your name, birth date, and ID, making the images anonymous. All systems must also comply with strict privacy laws (like HIPAA and GDPR) to keep your information encrypted and secure.
4. Will using AI make my scan more expensive?
Generally, no. Currently, patients usually don’t pay extra for AI analysis; hospitals absorb the cost to improve safety and efficiency. While insurance companies are starting to cover specific high-tech AI procedures, for now, it is typically part of the standard care covered by your scan.
5. Can AI help reduce radiation from X-rays and CT scans?
Yes! This is one of AI’s best benefits. AI allows doctors to take “low-dose” scans (using significantly less radiation) and instantly reconstruct them into crystal-clear, high-definition images. This makes scans much safer, especially for children or patients who need frequent imaging.